December 2, 2020
December 2, 2020
Case Study: Virtual Pulmonary Rehab Drives Improved Outcomes in COPD
71% of COPD patients report improvement in shortness of breath after using at-home breathing techniques taught virtually on MyCOPDTeam
One silver lining of the pandemic is that it opened up the floodgates of experimentation with engaging patients virtually in order to improve their health outcomes. Now, several months into these experiments, we have some data to share on the effectiveness of one such test: offering pulmonary rehab instruction – virtually – to patients with chronic obstructive pulmonary disorder on MyCOPDTeam.
Pulmonary rehab works. It’s like having a personal trainer to help you strengthen your breathing muscles, and many COPD patients rave about how much it has helped them combat shortness of breath. When COVID-19 hit, however, most pulmonary rehab came to an abrupt stop around the world. It was considered non-essential and too risky to bring patients with a respiratory disease into the clinics where the instruction was offered.
In response, we quickly teamed with the Home Rehabilitation Network, led by Alexander Grichuhin, to produce four videos for MyCOPDTeam that guide members through techniques and tips they can use to strengthen breathing and maintain health. One example: a tutorial on pursed-lip breathing, which delivers more oxygen in any given breath. It was all about giving members actionable tips to manage their condition – at home – while many in-person appointments and support groups remain on pause.
The impact has proven remarkable. When we surveyed members 30 days after the videos went live, we were thrilled to find that 92% of those who’d seen the videos had tried the techniques – with 48% reporting they’d done so more than 10 times.
Then 90 days after the videos went live, we conducted a follow-up survey among a subset of the original respondents and found remarkable improvements in several key quality of life measures. Strikingly, 79% of respondents to the follow-on survey continued using the techniques and 67% of them had made the techniques a daily habit!
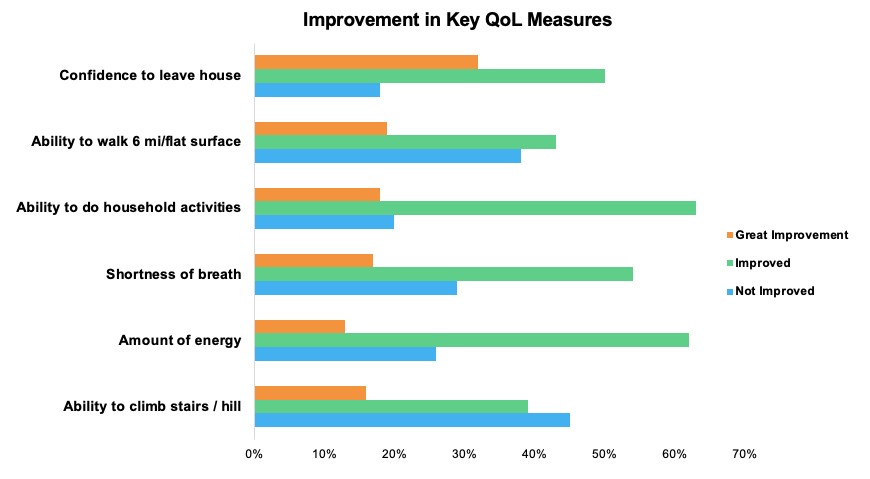
Regularly using the techniques learned from the videos led to improvements in six key quality of life measures.
82% report feeling more confident leaving their house. 81% see improvement in their ability to do household activities. 75% have more energy. 71% see improvements in shortness of breath. 62% are more comfortable walking for 6 minutes on a flat surface. 55% are better able to climb stairs or a hill. This kind of impact is so valuable, making it possible for people to more effectively, comfortably and safely do the things they want every day – at work, at home, for themselves and for their families.
It also underscores the importance of meeting patients where they are. Digital tools are playing such an important role in chronic condition care today. And listening to patients to understand what matters most to them – such as the ability to do “basic” household activities – is essential to addressing unmet patient needs and improving quality of life.
The positive response from patients is very clear: “We want more of this please!” We’re redoubling our commitment to creating and curating content that empowers people to play an active role in managing their health – during and beyond the continuing pandemic.
Have you seen similar approaches work well? Wondering how this approach might translate to a different condition or therapeutic area? We’d love to hear from you. Comment below or reach out to me at eric@myhealthteams.com.