 December 7, 2020
December 7, 2020
New Research: Women’s Real-World Experience with Endometriosis Pain, Treatments and Doctors
This year’s Congress of the Society of Endometriosis and Uterine Disorders (SEUD) featured a presentation from Oscar Antunez Flores, MD, Global and US Medical Affairs Director Women’s Health at AbbVie, based on research conducted among members of MyEndometriosisTeam led by MyHealthTeams’ senior research director, Beth Schneider. It was titled, “Women’s Perceptions on Endometriosis-related Pain Treatment and Interactions with Their Healthcare Providers.”
The findings revealed the striking gap between women’s daily pain and the effectiveness of available pain treatment. Three things that stuck with me after reviewing the research:
1) Endometriosis-related pain is intense – and persistent.
Among the 544 women surveyed, most from the U.S. and younger than 40, more than three quarters experience pain weekly. 54% of respondents experience pain daily.
2) Pain treatments are not yet effective enough for most women living with endometriosis – so they abandon them.
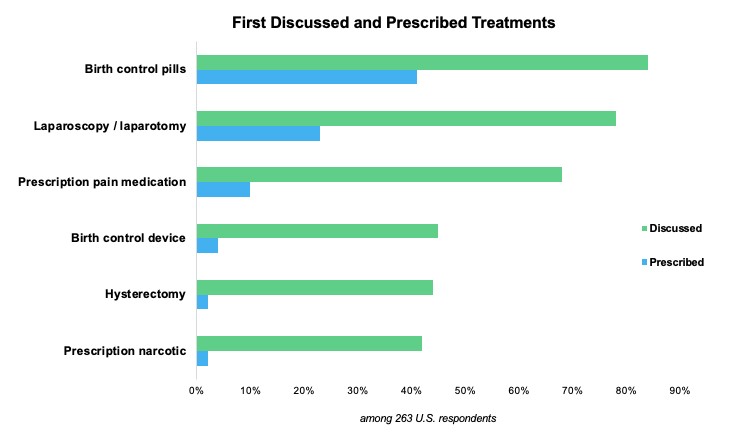
Our study found that doctor-patient conversations about potential treatments are fairly wide-ranging, with birth control pills, laparoscopy/laparotomy, and prescription pain medication being the most commonly recommended.
The majority of these women (57%) made their first treatment choice based on their doctor’s strong recommendation. About two-thirds of survey respondents, however, reported they discontinued their first endometriosis treatment because it did not relieve their pain. Another third discontinued their first treatment because of side effects.
Follow-up conversations with their doctors that led to second treatment decisions focused on a similar mix of options and had a similarly dismal impact. Approximately 45% of women surveyed reported they were “not at all satisfied or not very satisfied” with their second treatment for endometriosis-related pain.
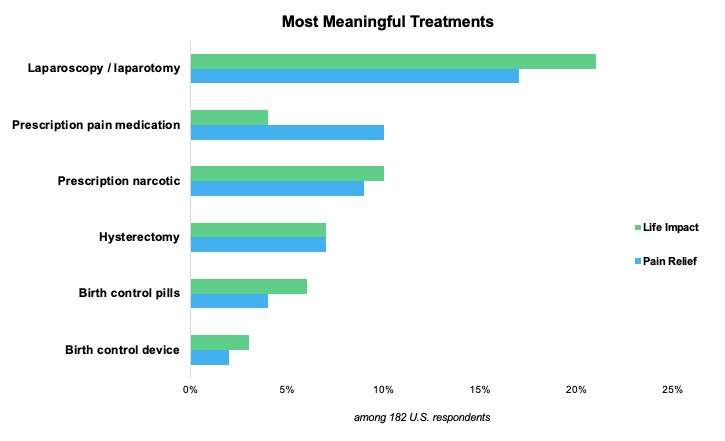
The women we surveyed reported that surgical procedures were among the most meaningful treatments for addressing their endometriosis-related pain. But too many women reported that no treatment was able to help their pain (16%) or improve their overall quality of life (19%).
The vast majority (89%) of these respondents have undergone at least one surgery in an attempt to alleviate their endometriosis-related pain. Nearly one in five has had four or more surgical procedures. And half (51%) have switched doctors through this treatment journey, primarily due to dissatisfaction with their doctor.
3) There is a big opportunity to improve women’s real-world experience with endometriosis pain, treatments and doctors.
Dr. Flores called out in his SEUD presentation that improved education for patients on endometriosis-related pain management and increased physician awareness of patients’ needs and goals may facilitate dialogue and help set clear pain management expectations. Indeed, our study found that the women who were most satisfied with their experience were also those most involved in treatment decision-making based on more detailed dialog with their doctors.
This focus on patient education that empowers women to have more productive conversations with their doctors is a top priority for our teams. Earlier this year, we teamed with AbbVie to launch the Endometriosis Resource Center, which provides actionable information for understanding the disease and discussing symptoms, treatments and more with doctors. We also produced a video Q&A with Dr. Georgine Lamvu to help members of our social network prepare for telehealth appointments and explore alternative treatment options while many elective surgeries were on hold due to COVID-19.
As we look ahead to 2021, we are committed to continuing to listen to women – conducting additional research that helps us identify unmet patient needs so we can best address patient priorities. Have you seen interesting new approaches to patient education that are proving successful? I’d love to hear about them. Comment below or find me at [email protected].