January 5, 2021
January 5, 2021
The Patient POV: The Impact of Lupus on Quality of Life
The American College of Rheumatology annual meeting featured research conducted among nearly 600 lupus patients on MyLupusTeam, our social network for people facing lupus.
The results point to an opportunity to improve the real-world experience of living with this condition. Four especially eye-opening takeaways:
1) Lupus symptoms are especially wide-ranging – taking a significant physical toll.
People facing lupus have many symptoms lying beneath the surface that greatly impact their quality of life. It’s not just the visible butterfly rashes that you may see on the face of a person with lupus, it is the invisible symptoms that take the greatest physical toll.
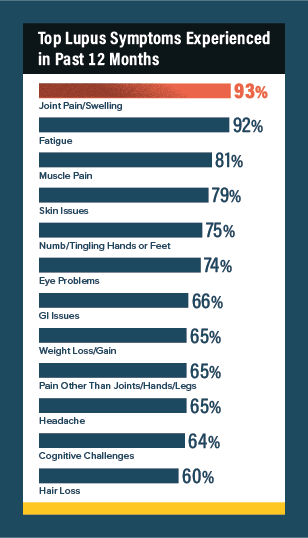
In the past 12 months, the top symptoms reported by the 593 survey respondents included:
- Joint pain/swelling (93%)
- Fatigue (92%)
- Muscle pain (81%)
- Skin issues (79%)
- Numb/tingling hands or feet (75%)
- Eye problems (74%)
Lupus, like many other autoimmune conditions, is similar to an iceberg in that the visible or known symptoms are just the tip of the iceberg poking out of the water. Many more significant symptoms lie beneath the surface – all of which need open discussion and treatment.
2) The physical toll of lupus translates into meaningful quality of life (QoL) impacts.
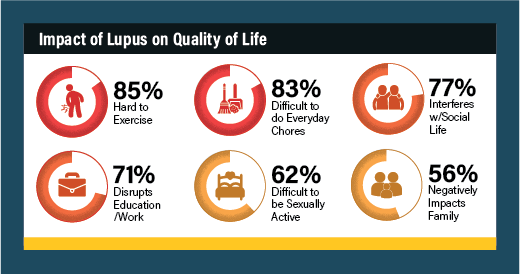
Accomplishing daily tasks and goals proves a formidable challenge for the vast majority of people living with lupus. Only about half of survey respondents report they feel they are able to live a “full life” because of the impact lupus has on their ability to exercise, be social, do chores, have sex, and work – among other things.
The top-reported quality of life impacts of lupus include:
- Hard to exercise (85%)
- Difficult to do everyday chores (83%)
- Interferes with social life (77%)
3) And the challenge of not fully living the life they want impacts mental health for many people facing lupus.
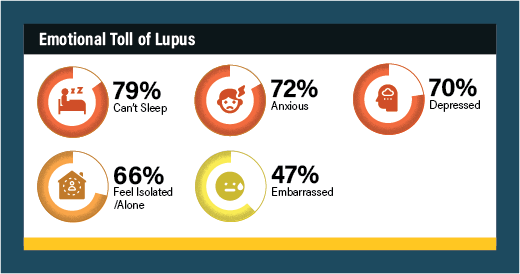
The emotional wallop of lupus is intense. 79% of survey respondents report extreme difficulty sleeping, 72% feel anxious, and 70% are depressed.
The unfortunate reality is there’s a vicious cycle happening here for people unable to get help. People facing lupus are living with severe pain and fatigue. This makes it hard to exercise and sleep, to accomplish goals at home or work, or to have fulfilling social and intimate relationships. So, naturally, people have a hard time feeling comfortable and confident, and connecting with others. It keeps compounding – and both the symptoms and their impact can get worse.
4) The obstacles to managing lupus point to an opportunity for patient education and engagement.
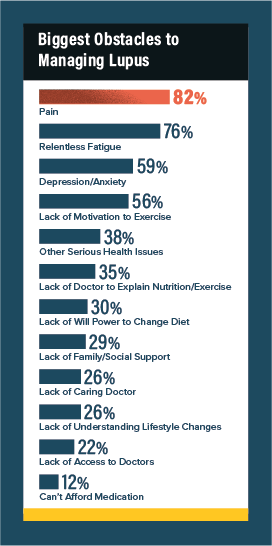
Members point to pain, fatigue and depression as serious obstacles to their being able to manage their lupus. In lieu of treatments that more or less put their lupus in remission (a goal that remains elusive for most people with lupus), effective pain management is critical to slowing the vicious cycle. Another less common but important theme is diet and exercise – which are challenging for many. The data show that people know they need to eat well and move frequently, but they often don’t know how to get started or lack the practical knowledge to stick with new healthy lifestyle habits over time. This is an area where digital resources play an important role – especially during COVID, when many appointments and in-person support groups are paused.
MyLupusTeam has more than 180,000 registered members, and the content we create and curate focused on practical tips for healthy habits always proves popular. Emotional support when kickstarting a new exercise routine goes a long way toward turning that into a habit. And people want trusted advice when starting a new eating plan – like our recent article, Lupus Diet and Nutrition: Foods to Eat and Avoid.
Ultimately, this is about helping people better manage their lupus – by empowering them with information and connections. To do that, we’ll continue to prioritize listening to our members so we understand their real-world experiences and can help address unmet patient needs.
As always, I welcome discussion about our research findings. Please comment below or reach me at [email protected].