 October 27, 2022
October 27, 2022
Understanding What Drives Lung Cancer Patients’ Satisfaction with Doctors and Treatments
With the five-year survival rate for early-detected, localized lung cancer now at 56%, people are living longer than ever before with this condition. Patients’ satisfaction with their oncologists is more nuanced than you might expect. A recent survey among members of MyLungCancerTeam, our social network for people living with lung cancer, featured in two poster sessions at this year’s World Conference on Lung Cancer, provides insights into how oncologists can increase patient satisfaction and how caregivers can better support people facing lung cancer.
Patient Satisfaction with Lung Cancer Care Team and Treatment Dynamics
For context, among the 117 MyLungCancerTeam members we surveyed, 55% are “very satisfied” with their physician care team – with another 22% “somewhat satisfied.” Taking a look at the differences between satisfied patients and those who are not very satisfied revealed stark differences in the degree to which a patient felt heard and empowered by their physician.
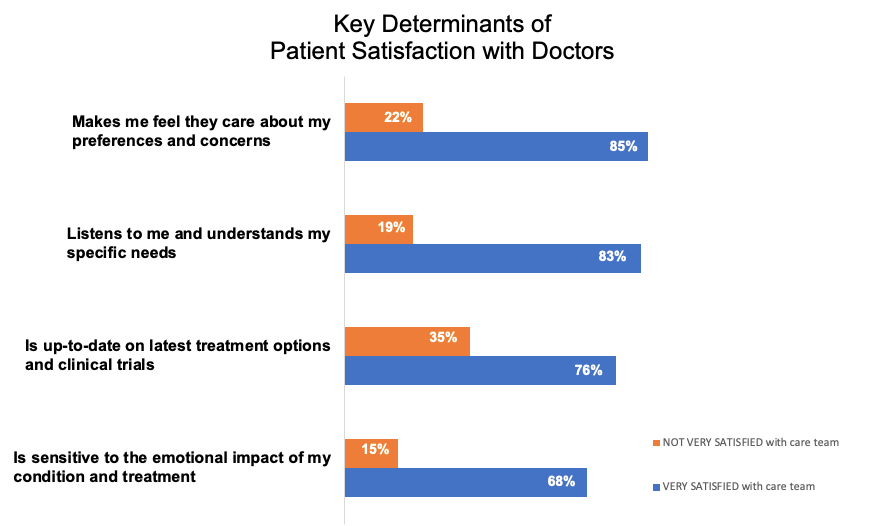
Notable findings include:
- 85% of those who are very satisfied agree their doctor “makes me feel they care about my preferences and concerns” (compared to only 22% of those who are not very satisfied).
- 83% of those who are very satisfied agree their doctor “listens to me and understands my specific needs” (compared to only 19% of those who are not very satisfied).
- 76% of those who are very satisfied agree their doctor “is up-to-date on latest treatment options and clinical trials” (compared to only 35% of those who are not very satisfied).
- 68% of those who are very satisfied agree their doctor “is sensitive to the emotional impact of my condition and treatment” (compared to only 15% of those who are not very satisfied).
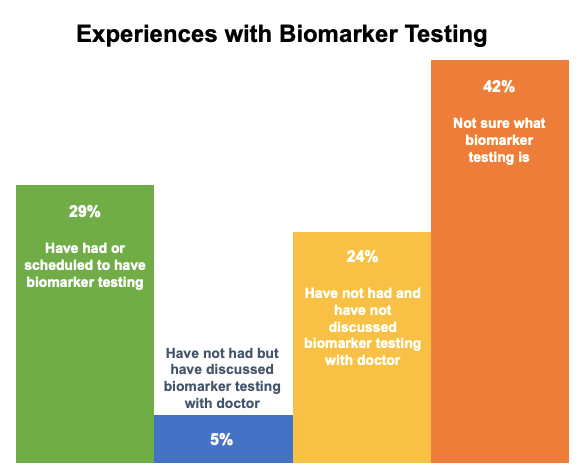
Need for Patient Education on Biomarker Testing
One important takeaway from this research is the need for additional patient education on biomarker testing – which can be critical to making the right treatment choice. Among those we surveyed, only 29% have had or are scheduled to have biomarker testing – while most have not discussed it with their doctors or are unsure what it is. This lack of awareness and access was especially pronounced among people with lower education levels, indicating an important opportunity to create more equity in lung cancer patient education and treatment offerings.
Impact of Lung Cancer Symptoms on Mental Health and Quality of Life
Understanding the importance of demonstrating sensitivity to the emotional impact of lung cancer is key – for doctors and caregivers alike. With its high mortality rate, being diagnosed with lung cancer takes a significant toll on mental health and quality of life.
- 73% of respondents agree with the statement “lung cancer makes me feel anxious.”
- 63% agree that “lung cancer makes me feel depressed.”
- 44% agree that “lung cancer makes me feel isolated or alone.”
But other factors beyond risk of mortality also play an important role in the mental health of patients.
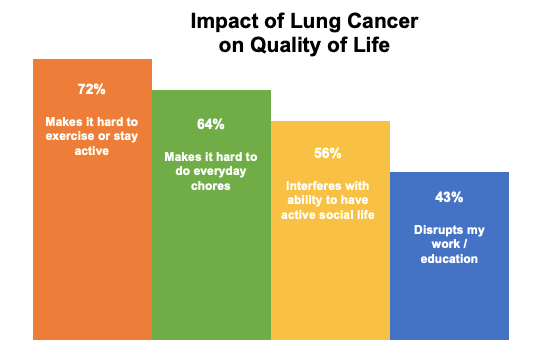
Survey respondents underscored that facing lung cancer makes “normal” life extremely difficult.
- 72% agree that “lung cancer makes it hard to exercise or stay active” – a critical ingredient to good mental health.
- 64% agree with the statement “lung cancer makes it hard to do everyday chores” – creating a loss of independence and autonomy.
- 56% agree that “lung cancer interferes with my ability to have an active social life” – many times friends and family don’t know how to interact with a person going through cancer and just avoid interacting with them.
- 43% agree that “lung cancer disrupts my work / education” – which can result in additional stress and a lost sense of purpose.
As one MyLungCancerTeam member put it, “So many things with cancer can get us depressed. It’s a big adjustment, just the fact we can’t do things we used to do.”
Additional Insights from the Patient POV
This research also explored topics including the steps people take and the biggest obstacles they face in managing lung cancer as well as gender differences in the real-world experience of living with lung cancer.
We’re happy to share the full findings of these surveys with you and your organization as well as share ideas on how to fill the patient education and care gaps these data reveal. These findings are very consistent with the research we have done with patients across the other 44 chronic condition communities we serve. To schedule time to discuss in more detail, please reach out to us at [email protected].
